Abstract
Background
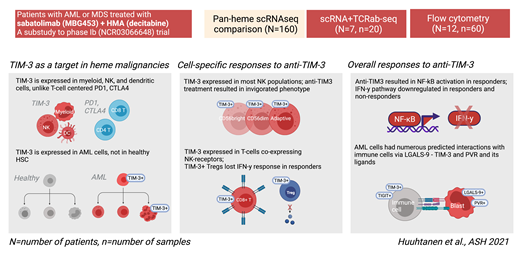
The success of allogeneic stem cell transplantation supports the notion that immunotherapy can have curative potential in AML, but immune checkpoint therapies (e.g., anti-PD1) have shown only modest clinical efficacy. TIM3 is an immune-checkpoint molecule expressed both on immune and leukemic cells but not on healthy hematopoietic stem cells (HSCs), making it a particularly interesting target in AML. In myeloid malignancies, the combination of anti-TIM3 therapy with hypomethylating agents (HMA), which may prime the tumor microenvironment for immune therapies, has shown promising initial response rates up to 50%-60% of patients, but their mechanism of action is not fully understood.
Methods
We analyzed the effects of anti-TIM3 (sabatolimab, MBG453) in combination with decitabine in 11 refractory/relapsed AML patients and 1 MDS patient recruited in a phase Ib trial (NCT03066648), with 5/12 responders (3 CR, 2 CRi). We studied paired bone-marrow (BM) and peripheral blood samples with scRNA+TCRαβ-seq enriched for CD45+ immune cells (90% of input) and blast cells (10%) and flow cytometry.
Additionally, to explore the expression of TIM3 and other immune checkpoints in different cell populations, we combined scRNAseq data from 160 BM aspirate samples across 10 different hematological malignancies and healthy controls.
Results
Our pan-heme scRNA-seq data analysis of over 500'000 cells revealed that unlike PD1 and CTLA4, HAVCR2 (TIM3) was primarily expressed in NK and myeloid cells (including dendritic cells [DCs], macrophages, and monocytes). In healthy controls, the expression of HAVCR2 was low in T-cells, but in patients with heme-malignancies, expression was seen on activated T-cells. In HSC populations, AML patients had generally upregulated HAVCR2 expression compared with healthy subjects.
ScRNAseq data of 20 samples (n=7 patients) treated with anti-TIM3+HMA revealed that at baseline, DCs were more highly represented in samples from the responding (n=4) than from the non-responding patients (n=3). Following anti-TIM3+HMA treatment, DCs expanded significantly, and upregulated pathways related to interleukin production (IL-1b, IL-18) in responders, suggestive of an activated inflammasome response.
At baseline, the most expanded NK-phenotype expressed the highest amounts of HAVCR2, which varied between patients from CD56 bright to adaptive NK cells. Anti-TIM3+HMA therapy modulated NK cells especially in responders, in which NK cells downregulated HAVCR2 and upregulated the NF-κB pathway. Importantly, the NF-κB pathway was upregulated in other cell types in responding patients, but not in non-responding patients. In contrast, the IFN-γ response was downregulated in both responding and non-responding patients in multiple different cell types.
The highest expression of HAVCR2 in T cells was seen in cells co-expressing NK-receptors and with the highest cytotoxicity. Analysis of the scTCRαβ-seq revealed that the combination treatment did not have a marked effect on T-cell clonality, but one patient with CR had a significantly expanded large granular lymphocyte (LGL) clone covering 4%-25% of the repertoire. In responding patients, HAVCR2+ regulatory T-cells were more numerous at baseline, contracted following therapy, and lost response to IFN-γ, a pattern not seen in non-responding patients.
The analysis of predicted cell-cell interactions between leukemic and immune cells did not show significant interactions between inhibitory PD1 or CTLA4, and their ligands, but ubiquitous LGALS9 - HAVCR2 interactions were predicted in leukemic bone marrows. Responding patients had more these interactions, which decreased following therapy. Non-responding patients had multiple interactions between T/NK cells and blasts via PVR and its ligands which were not seen in responding patients, which represent a putative resistance mechanism for anti-TIM3+HMA therapy.
Conclusions
Unlike PD1 and CTLA4, TIM3 is expressed on leukemic, DC, myeloid, and NK cells, and consistent with this finding, the effects of TIM3 blockade in vivo were mainly observed in these cell types. In responding patients, NFκB pathway was activated in T/NK cells following anti-TIM3 and HMA treatment concomitant with a decrease in inhibitory interactions. Our results pinpoint the differential effects of TIM3-blockade on immune cells and may aid in developing predictive biomarkers for treatment outcome.
Kreutzman: Novartis: Current Employment. Kontro: Astellas: Consultancy, Membership on an entity's Board of Directors or advisory committees; Jazz Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees; AbbVie: Membership on an entity's Board of Directors or advisory committees, Research Funding. Orlando: Novartis: Current Employment. Cremasco: Novartis: Current Employment. Wagner: Novartis: Current Employment, Current holder of individual stocks in a privately-held company. Pelletier: Novartis: Current Employment. Sabatos-Peyton: Novartis: Current Employment. Rinne: Novartis: Current Employment; Qiagen: Consultancy. Mustjoki: Janpix: Research Funding; Novartis: Research Funding; Pfizer: Research Funding; BMS: Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal